Pain is “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage
Types of PAIN
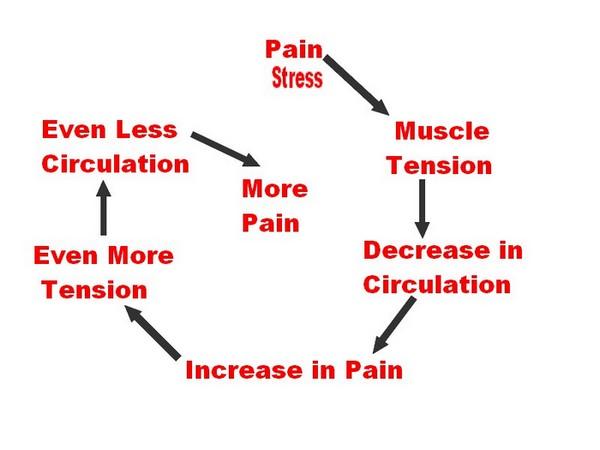
- Acute pain is caused by an injury to the body. It warns of potential damage that requires action by the brain, and it can develop slowly or quickly. It can last for a few minutes to six months and goes away when the injury heals.
- Chronic pain persists long after the trauma has healed (and in some cases, it occurs in the absence of any trauma). Chronic pain does not warn the body to respond, and it usually lasts longer than six months.
Cancer (or malignant) pain is associated with malignant tumors. Tumors invade healthy tissues and exert pressure on nerves or blood vessels, producing pain. Cancer pain can also be associated with invasive procedures or treatments. Some physicians classify cancer pain with chronic pain
PAIN BASED ON LEVEL OF STIMULATION
- SOMATIC PAINAssociated with skin and musculo-skeletal region Superficial and Deep
- VISCERAL PAIN Associated with viscera and internal organs
carried by un-myelinated type C fibers
INFLAMMATORY PAIN:
| Comparison between Acute and Chronic inflammation | ||
|---|---|---|
| Acute | Chronic | |
| Causative agent | Pathogens, injured tissues | Persistent acute inflammation due to non-degradable pathogens, persistent foreign bodies, or autoimmune reactions |
| Major cells involved | Neutrophils, mononuclear cells (monocytes, macrophages) | Mononuclear cells (monocytes, macrophages, lymphocytes, plasma cells), fibroblasts |
| Primary mediators | Vasoactive amines, eicosanoids | IFN-? and other cytokines, growth factors, reactive oxygen species, hydrolytic enzymes |
| Onset | Immediate | Delayed |
| Duration | Few days | Up to many months, or years |
| Outcomes | Resolution, abscess formation, chronic inflammation | Tissue destruction, fibrosis, necrosis |
| Name | Produced by | Description |
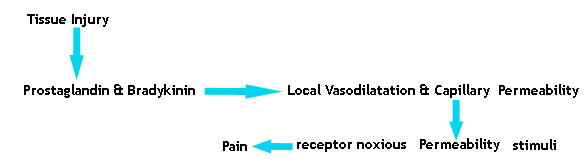
| Bradykinin | Kinin system | A vasoactive protein which is able to induce vasodilation, increase vascular permeability, cause smooth muscle contraction, and induce pain. |
| C3 | Complement system | Cleaves to produce C3a and C3b. C3a stimulates histamine release by mast cells, thereby producing vasodilation. C3b is able to bind to bacterial cell walls and act as an opsonin, which marks the invader as a target for phagocytosis. |
| C5a | Complement system | Stimulates histamine release by mast cells, thereby producing vasodilation. It is also able to act as a chemoattractant to direct cells via chemotaxis to the site of inflammation. |
| Factor XII (Hageman Factor) | Liver | A protein which circulates inactively, until activated by collagen, platelets, or exposed basement membranes via conformational change. When activated, it in turn is able to activate three plasma systems involved in inflammation: the kinin system, fibrinolysis system, and coagulation system. |
| Membrane attack complex | Complement system | A complex of the complement proteins C5b, C6, C7, C8, and multiple units of C9. The combination and activation of this range of complement proteins forms the membrane attack complex, which is able to insert into bacterial cell walls and causes cell lysis with ensuing death. |
| Plasmin | Fibrinolysis system | Able to break down fibrin clots, cleave complement protein C3, and activate Factor XII. |
| Thrombin | Coagulation system | Cleaves the soluble plasma protein fibrinogen to produce insoluble fibrin, which aggregates to form a blood clot. Thrombin can also bind to cells via the PAR1 receptor to trigger several other inflammatory responses, such as production of chemokines and nitric oxide. |
| Name | Type | Source | Description |
| Lysosome granules | Enzymes | Granulocytes | These cells contain a large variety of enzymes which perform a number of functions. Granules can be classified as either specific or azurophilic depending upon the contents, and are able to break down a number of substances, some of which may be plasma-derived proteins which allow these enzymes to act as inflammatory mediators. |
| Histamine | Vasoactive amine | Mast cells, basophils, platelets | Stored in preformed granules, histamine is released in response to a number of stimuli. It causes arteriole dilation and increased venous permeability. |
| IFN-? | Cytokine | T-cells, NK cells | Antiviral, immunoregulatory, and anti-tumour properties. This interferon was originally called macrophage-activating factor, and is especially important in the maintenance of chronic inflammation. |
| IL-8 | Chemokine | Primarily macrophages | Activation and chemoattraction of neutrophils, with a weak effect on monocytes and eosinophils. |
| Leukotriene B4 | Eicosanoid | Leukocytes | Able to mediate leukocyte adhesion and activation, allowing them to bind to the endothelium and migrate across it. In neutrophils, it is also a potent chemoattractant, and is able to induce the formation of reactive oxygen species and the release of lysosome enzymes by these cells. |
| Nitric oxide | Soluble gas | Macrophages, endothelial cells, some neurons | Potent vasodilator, relaxes smooth muscle, reduces platelet aggregation, aids in leukocyte recruitment, direct antimicrobial activity in high concentrations. |
| Prostaglandins | Eicosanoid | Mast cells | A group of lipids which can cause vasodilation, fever, and pain. |
| TNF-a and IL-1 | Cytokines | Primarily macrophages | Both affect a wide variety of cells to induce many similar inflammatory reactions: fever, production of cytokines, endothelial gene regulation, chemotaxis, leukocyte adherence, activation of fibroblasts. Responsible for the systemic effects of inflammation, such as loss of appetite and increased heart rate. |
Inflammation is a response of a tissue to injury, often injury caused by
invading pathogens. It is characterized by
- increased blood flow to the tissue causing
- increased temperature,
- redness,
- swelling, and
- pain
- Burns
- Chemical irritants
- Frostbite
- Toxins
- Physical injury, blunt or penetrating
- Immune reactions due to hypersensitivity
- Ionizing radiation
- Foreign bodies, including splinters, dirt and debris
- Trauma